|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Lesson 8 |
19-20th Centuries. Specialisations. Malaria. Chemotherapy. Antibiotics. The latest discoveries. Giuseppe Brotzu and cephalosporin. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
By the end of the 19th century surgery had taken gigantic steps forward, and in fact, there was now an anatomical underpinning, and anaesthesia had come into being, along with the concept of sepsis, but one important component was still lacking: monitoring the condition of the patient during surgery. In fact, when the surgeon operated on a patient under anaesthesia it was not known whether the latter was about to die or not. In that period (late 19th century) humanity was afflicted by various infective diseases among which were Yellow Fever and Malaria. It is worthy of note that in Sardinia the population was more resistant to Malaria because there was a high percentage of hereditary erythrocytemic carriers whose erythrocytes were resistant to plasmodium infection. On the other hand, colonisers coming from the mainland were not protected and were decimated by Malaria so few groups managed to establish themselves in Sardinia; except for the inhabitants of the island of Carloforte, the Greeks, and the inhabitants of the Padus Basin, all originating from areas of endemic Malaria among which hereditary erythrocytemia was widespread.
In Sardinia malaria was eradicated only in 1950 by the Rockefeller Foundation, which employed 30,000 men for 4 years, to launch out a massive campaign of land drainage and reclamation using the insecticide DDT. The operation's headquarters were situated in Cagliari at the Riva Villasanta school in Piazza Garibaldi. (See memorial plate) Among the epoch's other illnesses were: - Pellagra: although the existence of vitamins had not yet been discovered, the beginnings of an understanding of the fundamental cause of this disease, first described by Francesco Frapolli in 1771 and widespread in the plains of Lombardy-Veneto, had developed. It was in some way connected with the mono-diet based on maize. This disease, which brought grave complications to the nervous system, was eradicated when a varied diet containing the necessary vitamins was introduced. - "Miner's anaemia": this illness afflicted many workers employed in great public construction projects at the end of the 19th century (for example, the Gottardo and Saint Bernard Tunnel). It is a disease caused by the hematophagous parasite Ancylostoma duodenale (discovered by Angelo Dubini, 1813-1902) which lives in hot humid environments and entered into the miner's bodies through the skin of their bare feet. This disease also was widespread in the south of the USA where it became known as "Hookworm disease".
Another great discovery at the start of the 20th century, important to both medicine and surgery, was the discovery of the blood groups by the Austrian doctor Karl Landsteiner (1868-1943). Finally it was understood why the blood of different subjects was incompatible. In 1940, in cooperation with the American Alexander Wiener, he discovered the Rh factor as well. Great discoveries also were made in the field of bacteriology at the beginning of the 20th century. The diphtheria bacillus was identified and several vaccines were developed. In 1905 the German Fritz Richard Schaudinn (1871-1906) identified Treponema pallidum, the aetiological agent of syphilis which was widespread until then, making this an epoch-making discovery. Some years later in 1910 an excellent bacteriologist, Paul Ehrlich (1854-1915), for the first time perfected a synthetic pharmaceutical drug (chemotherapy) capable of attacking a germ: in this case the spirochete Treponema pallidum. He noticed that certain colorants bonded with the bacteria from which he got the idea of finding a substance which would bind to the bacteria and kill it. In cooperation with the Japanese Sahachiro Hata (1873-1938) he tried 605 compounds before finding one based on arsenic which was effective. He called it Salvarsan, 606. Being toxic, it was substituted by the less toxic Neosalvarsan. In the meantime women had entered the scientific scene: First women to be awarded a degree:
- Elena Cornaro Piscopio, Padua 1678; Female M.Ds in the world:
- Miranda Stuart (alias James Barry), Edinburgh 1812 Female M.Ds in Italy:
- Ernestina Paper in Florence 1877 (originally from Odessa). First year in Zurich (where the first female doctor graduated in 1867) Female M.Ds in Sardinia:
- Paola Satta, Cagliari, 1902
Some years late, in 1935, Gerhard Domagk (1895-1964), a student of Ehrlich, by starting with a derivative of aniline discovered prontosil-rubrum, precursor of a class of chemotherapeutic drugs: the sulphamides. In a time when infectious diseases decimated the population to such an extent that life expectancy was about 40 years, the sulphamides become very important. Moreover, they were immediately produced everywhere on a large scale because they were based on aniline, a molecule that was under international patent since many years. Some time later, a group of scientists at the Pasteur Institute in Paris, among whom were Federico Nitti (1905-1947) and Daniel Bovet (1907-1992), discovered the reason why the sulphamides were effective in vivo and not in vitro (in culture): in order to be effective it was necessary for one part of the molecule to be removed when the drug entered the organism. Daniel Bovet, who later became profesor of Pharmacology at the University of Sassari, was awarded the Nobel prize in 1957 for his work on antihistamines.
After penicillin, another antibiotic was discovered by Selman Abraham Wacksman (1888-1973) in 1944: streptomycin. This drug was effective against tubercular mycobacteria and even though it is toxic to an extent, it is still used today. These were years in which great medical progress was made. Margaret Sanger (1879-1966) was born in a time when contraceptives were criminalized in almost all the world. One of eleven children born to a working class Irish Catholic family in Corning, New York, at 19 years Margaret saw her 50 years old mother die of tuberculosis, following eleven childbirths and seven miscarriages. Trained as a nurse in New York, Margaret Sanger devoted her life to legalizing birth control and making it universally available for women. In 1914 she coined the term "birth control" and soon began to provide women with informations and contraceptives. After having been repeatedly arrested and indicted, in 1921 she founded the American Birth Control League and spent her next three decades campaigning to make available a safe and effective birth control. By the 1950s, however, although she had won many legal victories, Sanger was far from happy with the limited birth control options available to women. By a matter of facts, since the 1842 invention of the diaphragm in Europe and the introduction of the first full-length rubber condom in 1869, there had been no new advances in contraceptive methods. Since 1912 she had been dreaming of a "magic pill" for contraception that could provide women with cheap, safe, effective and female-controlled contraception. Her search ended in 1951 when she met Gregory Goodwin Pincus (1903-1967), a medical expert in human reproduction who had been expelled from the University of Harward for having published a book on the in vitro fertilization of rabbit eggs, who was willing to take on the project and was searching for funds. Soon after, she found a sponsor in her rich friend Katharine McCormick (1875-1967) one of the first female ever graduated in technology. In the synthesis of hormones Pincus was aided by research chemists Russell Marker and Carl Djerassi; the clinical experimentation was carried in Puerto Rico by a catholic physician, John Rock (1890-1984). Their collaboration would lead in 1960 to the first oral contraceptive (Enovid). In Italy birth control was approved only in 1971. George Papanicolau (1883-1962) perfected a method for colouring and collecting vaginal strips (the Pap-test); so thanks to him prevention of tumours in the uterine cervix made "huge steps forward". The discovery of Sickle Cell Anaemia (the first molecular disease) caused by mutation of an amino acid in the Hb protein chain (Linus Pauling 1901-1994).
In addition, during the 1960s transplanting organs (see tables) became a possibility. The pioneer of this type of operation (in the early 20th century) was a French scientist who settled in America, Alex Carrel (1873-1944) who managed to keep human cells alive on a plate and then attempted transplants on animals. The first heart transplant was carried out in South Africa by Christian Barnard (1922-2001) in 1967. Unfortunately Barnard's attempts failed because Cyclosporin was not available (it was introduced in 1978 thanks to Jean Borel) so these patients only survived for a short period after the transplant. Cyclosporin is a drug which induces immuno-suppression thus impeding the likelihood of the new organ being rejected (that is, the new organ being attacked by the recipient's immune system). The first heart transplant to take place in Italy was carried out by Vincenzo Gallucci (1935-1991) in 1985 in Padova, and the second by Mario Viganò in the same month of the same year in Pavia. Mario Viganò also carried out both the first heart-lung transplant and the first permanent artificial heart implant in Italy. The first liver transplant was carried out in Colorado in 1967 and by Raffaello Cortesini in Italy in 1982. In Sardinia transplants of Bone marrow, Heart, Kidney and Liver are currently performed both in Cagliari and in Sassari.
the list refers to successful organ allotransplantations and associated accessory techniques in humans
Note: The list concerning transplants both in the world and in Italy is incomplete and arbitrary owing to the difficulty of collecting and verifying the relevant data. In Sardinia organ transplants (bone marrow, heart, kidney and liver) are carried out both in Cagliari and in Sassari. However, it must not be forgotten that notwithstanding the great progress made, some infectious diseases still were widespread, one of which was poliomyelitis caused by the polio virus (it is sufficient to remember that a whole wing of the paediatric hospital of Cagliari was given over to polio victims). Poliomyelitis was a devastating disease as it destroyed the medullar alpha motoneurons causing flaccid paralysis, atrophy of the muscular tissue which was replaced with connective tissue, and problems in bone formation. This disease was eradicated thanks to a vaccine developed (with dead germs) in America by Jonas Edward Salk (1914- 1995) in 1955, ten years after polio victim President Roosevelt had passed away. The vaccine was immediately used on a large scale, but, unfortunately, there were serious complications because some germ cell types were not killed and, once injected, caused the very disease, poliomyelitis, that they were supposed to prevent. Later Albert Bruce Sabin (1906-1993), introduced the oral vaccination (which was introduced in Italy at the beginning of the 1970s). This vaccine is prepared as a live attenuated strain that embeds itself in the intestinal mucosa where it replicates and having lost most of its neurotropism, does not usually produce complications in the nervous system. After a period when both types of vaccine were used, the one still employed is that of Salk. The Discovery of Cephalosporin * During fascist times, Brotzu had already been involved in the fight against malaria. After the war he was a consultant to the Rockefeller Foundation which, thanks to land reclamation and the massive use of DDT, succeeded in eradicating malaria (1950) by eliminating its carrier. Notwithstanding his great merits (for having discovered the cephalosporium he was proposed for the Nobel Prize) he is not usually mentioned in Italian texts, whereas, in contrast, he is named in pharmacological textbooks throughout the world. Brotzu received neither honour, nor money. In fact, he consigned several strains of cefalosporium fungus to an English sanitary official who had come to Sardinia in the anti-malaria campaign. In turn, this official gave the material to Edward Abraham (1913-1999), a student of Fleming, who isolated the cephalosporin. The drug was then sold throughout the world by the pharmaceutical companies Glaxo and Lilly making an enormous profit for them. During these lessons the way in which the concept of "Medicine" has changed through the centuries has been seen. Initially holistic conceptualisations predominated that placed man at the centre of everything (because it was no possible to define the diseases and their causes). Successively, especially from Morgagni onwards, medicine passed to a reductionist conceptualisation (from the study of the organ, to the tissue, to the cell, to the molecule). This has brought about an increased specialisation that while positive, has placed the disease at its centre rather than humankind. It is necessary to consider the organism itself, the human in his or her entirety as a microcosm composed of body and psyche. (* The notes on the discovery of cefalosporin are taken from the book by Paracchini R: "Il signore delle cefalosporine". Demos, Cagliari. 1992. Information of the first female M.D. in Sardinia come from the article by Enrico Fanni: Paola Satta la prima donna medico sarda. Bollettino Ordine dei Medici della Provincia di Cagliari, 6: 14-15, 2008) -------------------------------- To learn more: To learn more: ARMOCIDA G., ZANOBIO B. - Storia della Medicina. Masson, Milano 2003. BELLONI L. - Per la Storia della Medicina. Forni, Sala Bolognese, 1981. GRMECK M.D. (Ed). - Storia del Pensiero Medico Occidentale (3 Vol.). Laterza, Bari 1993-1996. KIPLE K.F. (Ed). - The Cambridge World History of Human Disease. Cambridge University Press, Cambridge, 1993, KENNEDY M.- A brief history of disease science and medicine. From the ice age to the genome project. Writers’ collective, Cranston, Rhode Island, 2004, NULAND SB. Doctors: The illustrated history of medical pioneers, Black Dog & Leventhal, 2008. RIVA A.. The Clemente Susini’s anatomical waxes in the university of Cagliari, 2002 http://pacs.unica.it/cere/home_en.htm. RIVA A. Flesh & Wax. The Clemente Susini’s anatomical models in the university of Cagliari. Ilisso, Nuoro 2007. http://www.ilisso.it. WAGNER LN. A history of medicine 2nd Ed, Informa N.York, 2007.
Considering just the Italian literature, further interesting information on the subject are found in the texts authored by: Further readings on the History of Medicine in Sardinia: CASTALDI L. - Francesco Boi, primo cattedratico di anatomia umana a Cagliari e le Cere fiorentine di Clemente Susini. Leo S. Olschki, Firenze, 1947. CATTANEO L., RIVA A. - Le Cere Anatomiche di Clemente Susini dell'Università di Cagliari. Bilingual Edition with English text. Edizioni Della Torre, Stef, Cagliari, 1993. DEL PIANO L (a cura di) - Per Giuseppe Brotzu-Dedicated to G. Brotzu. Edizioni Della Torre, Cagliari, 1998. DODERO G. - Storia della medicina e della sanità pubblica in Sardegna. Aipsa, Cagliari, 1999. DODERO G. - I Lazzaretti, epidemie e quarantene in Sardegna. Aipsa. Cagliari, 2001 FANNI G. - Sebastiano Perra (Sinnai 1772-Cagliari 1826). Un medico ippocratico nell'Ottocento cagliaritano. Contributo alla conoscenza dela Storia della Medicina sarda. Aipsa, Cagliari, 2002. MANCONI F. - Castigo de Dios. Donzelli, Roma 1994. RIVA A. Flesh & Wax. The Clemente Susini’s anatomical models in the university of Cagliari. Ilisso, Nuoro 2007. http://www.ilisso.it. RIVA A. Le cere anatomiche di Clemente Susini dell’Università di Cagliari. http://pacs.unica.it/cere/. ROCCHINI G.F. - Strumenti Medico-Chirurgici. http://www.amber-ambre-inclusions.info/it-strumenti_medici.htm TOGNOTTI E. - Americani, comunisti e zanzare: il piano di eradicazione della malaria in Sardegna tra scienza e politica negli anni della ella guerra fredda (1946-1950). EDES, Sassari, 1995. TOGNOTTI E. - Il mostro asiatico. Storia del colera in Italia. Laterza, Bari, 2000. TOGNOTTI E. - La spagnola in Italia: storia dell'influenza che fece temere la fine del mondo, 1918-1919. F.Angeli, Milano, 2002. VALENTI C., TORE G. (a cura di ) - Sanità e Società. Sicilia e Sardegna secoli XVI-XX. Casamassima, Udine, 1988. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
From the notes of Ramona Stara |
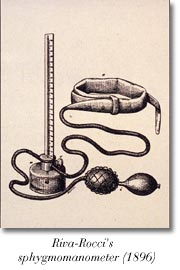 The person who invented the equipment to monitor the patient was Scipione Riva-Rocci (1863-1937) a student of Carlo Forlanini (1847-1918), who, in 1896, used simple objects (an ink-pot, mercury, a bicycle tubular tire) to construct a piece of equipment that, because of its small size and handiness, could be used in the operating theatre or by the duty doctor. In fact, instruments to measure blood pressure had already been invented, but they were very cumbersome and difficult to use. The sphygmomanometer was then perfected by the discovery of the cardiac tones discovered by the Russian Nicolaj Sergievich Korotkov (1874-1920) that allowed to measure minimum arterial pressure as well. Riva-Rocci's sphygmomanometer interested Harvey Cushing (1869-1939), a famous American neurosurgeon, who came to Italy specifically to meet him and to see the instrument of which he personally made a drawing. Cushing took the sphygmomanometer back to America with him and, from there, its use spread throughout the world.
The person who invented the equipment to monitor the patient was Scipione Riva-Rocci (1863-1937) a student of Carlo Forlanini (1847-1918), who, in 1896, used simple objects (an ink-pot, mercury, a bicycle tubular tire) to construct a piece of equipment that, because of its small size and handiness, could be used in the operating theatre or by the duty doctor. In fact, instruments to measure blood pressure had already been invented, but they were very cumbersome and difficult to use. The sphygmomanometer was then perfected by the discovery of the cardiac tones discovered by the Russian Nicolaj Sergievich Korotkov (1874-1920) that allowed to measure minimum arterial pressure as well. Riva-Rocci's sphygmomanometer interested Harvey Cushing (1869-1939), a famous American neurosurgeon, who came to Italy specifically to meet him and to see the instrument of which he personally made a drawing. Cushing took the sphygmomanometer back to America with him and, from there, its use spread throughout the world. 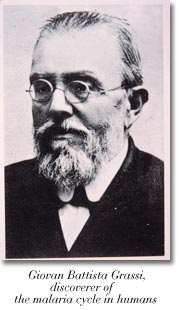 A student of Pasteur, Alphonse Laveran (1945-1922), discovered the aetiological agent of Malaria to which he gave the name "oscillatorium malariae" (it was later named "Plasmodium" by the two Italian malariologists Ettore Marchiafava (1847-1935), and Angelo Celli (1857-1914)). Walter Reed (1851-1902) discovered the role played by a mosquito (Aedes aegypti) in the transmission of Yellow Fever, while the Englishman, Ronald Ross (1857-1932)demonstrated the malaria cycle in birds. In fact, it was Giovanni Battista Grassi (1854-1925), who made the most important contribution to understanding the biological cycle of the parasite in man as he identified the mosquito of the Anopheles genus. However, for political reasons the Nobel Prize was given to Ross.
A student of Pasteur, Alphonse Laveran (1945-1922), discovered the aetiological agent of Malaria to which he gave the name "oscillatorium malariae" (it was later named "Plasmodium" by the two Italian malariologists Ettore Marchiafava (1847-1935), and Angelo Celli (1857-1914)). Walter Reed (1851-1902) discovered the role played by a mosquito (Aedes aegypti) in the transmission of Yellow Fever, while the Englishman, Ronald Ross (1857-1932)demonstrated the malaria cycle in birds. In fact, it was Giovanni Battista Grassi (1854-1925), who made the most important contribution to understanding the biological cycle of the parasite in man as he identified the mosquito of the Anopheles genus. However, for political reasons the Nobel Prize was given to Ross.  In 1895 the German physicist Wilhelm Konrad Roentgen (1845-1913) accidentally discovered that the rays from a cathode ray tube could pass through the bones of the skeleton and leave an impression on a photographic plate or on a fluorescent screen. Thus radiology was born (the first radiography taken by him was of his wife's hand and went around the world). Obviously the unrestrained use of X-rays without any protection, affected the doctors who thus used it badly since they were unaware that it would cause lesions (many radiologists died of radiodermatitis or from tumours). Great progress in radiography was then made by the American Walter Canon (1871-1945) who introduced the use of methods of contrast which allowed otherwise invisible organs to be seen. Then, gradually, new techniques were perfected such as echography (which uses ultra-sound - ultrasonography) after which followed TAC (computerised tomography CT) and Nuclear Magnetic Resonance Imaging (MRI).
In 1895 the German physicist Wilhelm Konrad Roentgen (1845-1913) accidentally discovered that the rays from a cathode ray tube could pass through the bones of the skeleton and leave an impression on a photographic plate or on a fluorescent screen. Thus radiology was born (the first radiography taken by him was of his wife's hand and went around the world). Obviously the unrestrained use of X-rays without any protection, affected the doctors who thus used it badly since they were unaware that it would cause lesions (many radiologists died of radiodermatitis or from tumours). Great progress in radiography was then made by the American Walter Canon (1871-1945) who introduced the use of methods of contrast which allowed otherwise invisible organs to be seen. Then, gradually, new techniques were perfected such as echography (which uses ultra-sound - ultrasonography) after which followed TAC (computerised tomography CT) and Nuclear Magnetic Resonance Imaging (MRI). 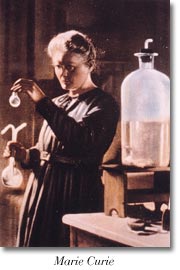 - the physicist Marie Curie (1867-1934) who won two Nobel prizes, one for physics and one for chemistry, for her discoveries with radiation which were immediately applied to curing tumours.
- the physicist Marie Curie (1867-1934) who won two Nobel prizes, one for physics and one for chemistry, for her discoveries with radiation which were immediately applied to curing tumours. 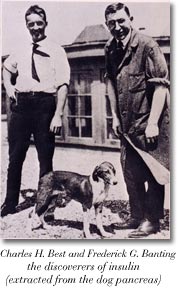 In the light of new discoveries, at the beginning of the 20th century a great many sciences flourished including vitaminology and above all endocrinology, whose founder was Charles E. Brown Sequard (1817-1894). The most important discoveries in this field were made in the 1920s by Charles H. Best (1899-1978), Frederick G. Banting (1891-1941) and John J. Mac Leod (1876-1935) in Toronto (the two latter physicians were awarded the Nobel prize for this work in 1923). They discovered that diabetes, a widespread disease and fatal at that time, could be cured with insulin, a hormone produced by the pancreas, and which could be extracted from the pancreas.
In the light of new discoveries, at the beginning of the 20th century a great many sciences flourished including vitaminology and above all endocrinology, whose founder was Charles E. Brown Sequard (1817-1894). The most important discoveries in this field were made in the 1920s by Charles H. Best (1899-1978), Frederick G. Banting (1891-1941) and John J. Mac Leod (1876-1935) in Toronto (the two latter physicians were awarded the Nobel prize for this work in 1923). They discovered that diabetes, a widespread disease and fatal at that time, could be cured with insulin, a hormone produced by the pancreas, and which could be extracted from the pancreas.  Meanwhile, the first antibiotic penicillin was discovered in 1928. The British bacteriologist Alexander Fleming (1881-1955) discovered that on a Petri dish he had left near a window, areas of inhibition had formed in which germs had not grown. He deduced that there must have been something blocking the growth of the microrganisms, so he asked a colleague to analyse the culture and a fungus was found. However, he was mistaken in his initial analysis for instead of "Penicillum notatum" (which inhibited the growth of bacteria) he identified another, ineffective, Penicillum. Fleming noticed the error, and published the work on Penicillum notatum which, however, was then only used to clean bacteriological cultures rather than as a pharmaceutical drug. In the Second World War it became necessary to find a drug to fight at least some of the numerous infections, so under the auspices of both the British and the American governments the Jewish chemist of German origin Boris Chain (1906-1979), and the Australian doctor Howard Florey (1898-1968), worked together to make penicillin a pharmaceutical drug. They were employed for an enormously important purpose and they began to produce penicillin in Britain and in America on a large scale as soon as possible (1941). However, it became an Allied monopoly, so to obtain it in Italy, at that time, "gold" had to be paid on the black market.
Meanwhile, the first antibiotic penicillin was discovered in 1928. The British bacteriologist Alexander Fleming (1881-1955) discovered that on a Petri dish he had left near a window, areas of inhibition had formed in which germs had not grown. He deduced that there must have been something blocking the growth of the microrganisms, so he asked a colleague to analyse the culture and a fungus was found. However, he was mistaken in his initial analysis for instead of "Penicillum notatum" (which inhibited the growth of bacteria) he identified another, ineffective, Penicillum. Fleming noticed the error, and published the work on Penicillum notatum which, however, was then only used to clean bacteriological cultures rather than as a pharmaceutical drug. In the Second World War it became necessary to find a drug to fight at least some of the numerous infections, so under the auspices of both the British and the American governments the Jewish chemist of German origin Boris Chain (1906-1979), and the Australian doctor Howard Florey (1898-1968), worked together to make penicillin a pharmaceutical drug. They were employed for an enormously important purpose and they began to produce penicillin in Britain and in America on a large scale as soon as possible (1941). However, it became an Allied monopoly, so to obtain it in Italy, at that time, "gold" had to be paid on the black market. 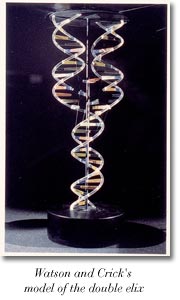 The discovery of the double helix model of DNA (James Dewey Watson, 1928-2004, and Francis Harry C. Crick, 1916-1953). Another important discovery was that of neurotransmitters (Julius Axeroldv, Ulf Svante von Euler, and Bernard Katz).
The discovery of the double helix model of DNA (James Dewey Watson, 1928-2004, and Francis Harry C. Crick, 1916-1953). Another important discovery was that of neurotransmitters (Julius Axeroldv, Ulf Svante von Euler, and Bernard Katz).  Furthermore, it is thanks to the Italian scientist Rita Levi Montalcini that the Nerve Growth Factor was discovered. NGF is important in the prevention of certain diseaeses such as Alzheimers. It was a discovery that was to win her the Nobel Prize for medicine
Furthermore, it is thanks to the Italian scientist Rita Levi Montalcini that the Nerve Growth Factor was discovered. NGF is important in the prevention of certain diseaeses such as Alzheimers. It was a discovery that was to win her the Nobel Prize for medicine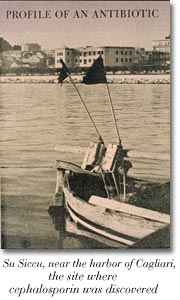 The Professor of Hygiene of the University of Cagliari, Giuseppe Brotzu (1895-1976), wondered why typhoid fever was less virulent in his city than elsewhere. He had formulated various hypotheses, all in vain. One day, while he was passing through the neighbourhood of the bay of "Su Siccu" he saw some young people bathing in the sea , just in the waters where Cagliari sewer system debouches without contracting the disease.
The Professor of Hygiene of the University of Cagliari, Giuseppe Brotzu (1895-1976), wondered why typhoid fever was less virulent in his city than elsewhere. He had formulated various hypotheses, all in vain. One day, while he was passing through the neighbourhood of the bay of "Su Siccu" he saw some young people bathing in the sea , just in the waters where Cagliari sewer system debouches without contracting the disease. 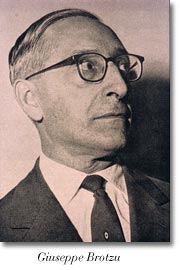 So he took a sample of the water to test its effect on a culture of Salmonella typhi. Since it was wartime and there was no meat to make the broth for the culture medium, Brotzu used the placentas obtained from parturient women in the maternity ward, that he then boiled in order to obtain the medium. With the help of his assistant Antonio Spanedda (1907-1998), he isolated a fungus from this water that produced an effective substance against Gram-negative bacteria- (the typhoid is in fact caused by Salmonella typhi, which like all the enterobacteriaceae is Gram- negative) however, the fungal extract he had prepared was a raw compound which could not be produced on a larges scale. When Brotzu asked for funding from the Italian Committee for research it was not given to him for political reasons since he had previously adhered to Fascism, as did almost all Italian university professors. Moreover, Brotzu dedicated himself less to research because he got more involved in politics, first becoming Mayor of Cagliari and then President of the Region of Sardinia.
So he took a sample of the water to test its effect on a culture of Salmonella typhi. Since it was wartime and there was no meat to make the broth for the culture medium, Brotzu used the placentas obtained from parturient women in the maternity ward, that he then boiled in order to obtain the medium. With the help of his assistant Antonio Spanedda (1907-1998), he isolated a fungus from this water that produced an effective substance against Gram-negative bacteria- (the typhoid is in fact caused by Salmonella typhi, which like all the enterobacteriaceae is Gram- negative) however, the fungal extract he had prepared was a raw compound which could not be produced on a larges scale. When Brotzu asked for funding from the Italian Committee for research it was not given to him for political reasons since he had previously adhered to Fascism, as did almost all Italian university professors. Moreover, Brotzu dedicated himself less to research because he got more involved in politics, first becoming Mayor of Cagliari and then President of the Region of Sardinia.